Our News

Join Spirit Health Foundation’s ‘Reach the Peak’ challenge to help save lives around the world
Spirit Health Foundation is calling on individuals and teams to take part in its Ben Nevis Fundraising Challenge 2025, ‘Reach the Peak’, from Friday 26 to Sunday 28 September 2025.
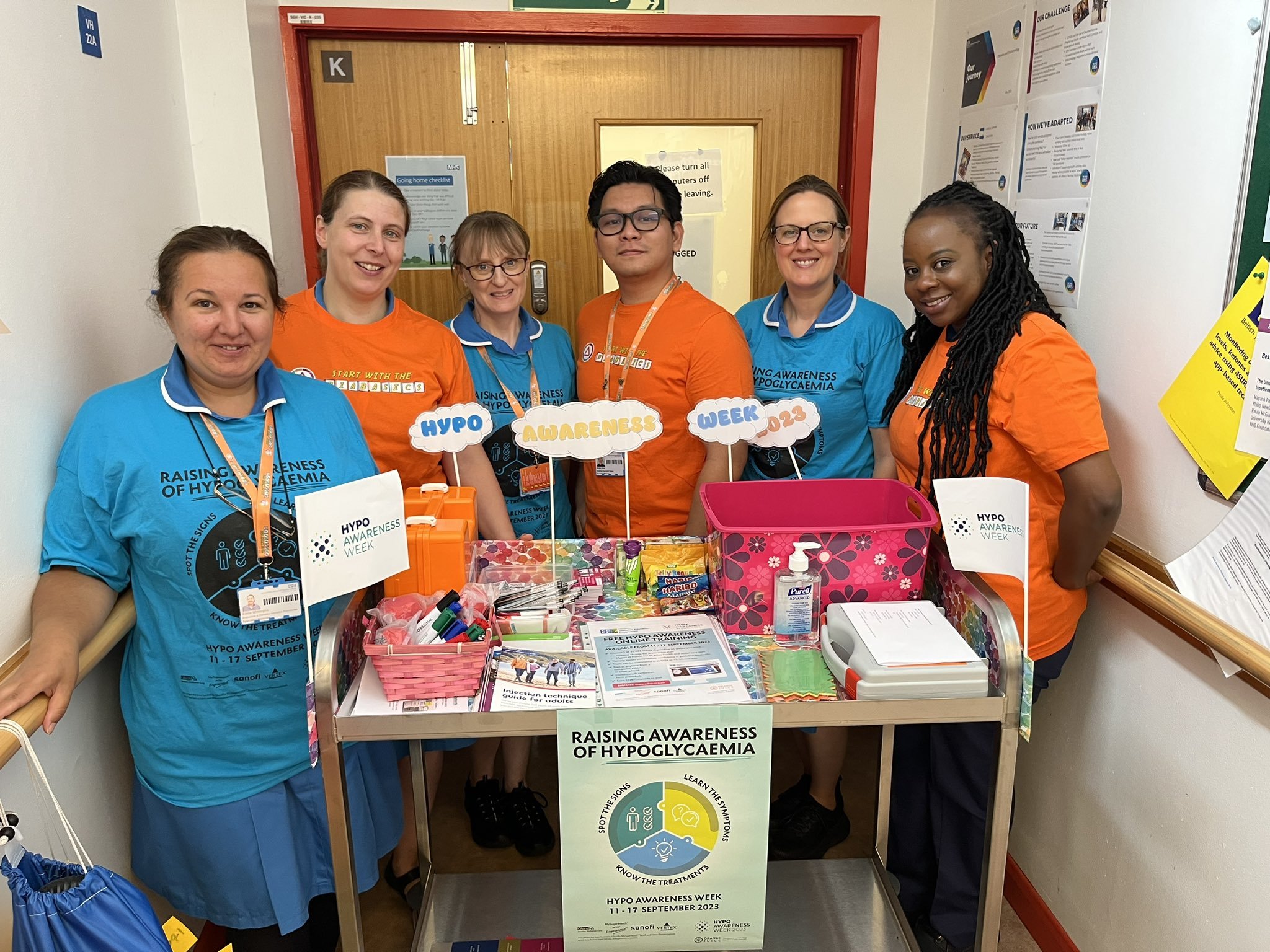
Registrations open for Hypo Awareness Week 2025
We anticipate we will receive pharmaceutical sponsorship for this event. As soon as the sponsorship is confirmed, the details will be added to the website and all promotional materials where appropriate.
Hypo Awareness Week is back from 6 to 12 October 2025, uniting healthcare professionals across the UK and Ireland to shine a spotlight on the risks of hypoglycaemia.

Diabetes nurse receives top accolade
A senior lead diabetes nurse manager from the Hywel Dda Health Board in Wales has been recognised for her contribution to improving patient care.

New anthem from girl band raises awareness of type 1 diabetes after research highlights silent struggle
Four talented teens living with autoimmune type 1 diabetes (aT1D) have come together to form a girl band named "1Type", Sanofi and Stagecoach Performing Arts have announced.

Stroke survivor regains independence thanks to simple diabetes innovation
A simple device has helped transform the life of 63-year-old Maureen, a stroke survivor who was left dependent on district nurses for daily insulin injections.

Positive data for zimislecel in type 1 diabetes presented at ADA 2025
Vertex presented updated data from the Phase 1/2 portion of the Phase 1/2/3 FORWARD-101 clinical trial of zimislecel during the American Diabetes Association 85th Scientific Sessions.

Winners announced at the Diabetes Nursing Awards 2025
The winners of the Diabetes Nursing Awards 2025 were revealed at a prestigious ceremony in London last week, celebrating excellence, innovation and dedication in diabetes care.

Registrations are now open for the webinar ‘Breaking new ground: Further development to transform diabetes and CKD care’
Led by Professor James Burton, a Professor of Renal Medicine and Honorary Consultant Nephrologist at the University of Leicester, the session will be held on June 24 at 12:30pm.

Spirit Health launches annual training award to recognise contributions to diabetes care
Spirit Health has launched its new Training Excellence Award, celebrating healthcare professionals who go above and beyond to support people living with diabetes through education and training.

Webinar to explore case studies in diabetes and kidney disease management
Healthcare professionals are invited to join a live webinar exploring the management of diabetes and kidney disease through engaging case studies.

New diabetes YouTube channel to provide free education
A free diabetes YouTube channel designed to provide valuable, accessible educational content has been launched.

Recent advances in diabetic neuropathy using rodent models
Join us for a free online webinar organised by NEUROdiab, the international Diabetic Neuropathy Study Group. Chaired by Doctor Stephanie Eid, the session will be held on Wednesday 11 June 2025, 6:00 PM – 7:15 PM (BST UK), 1:00 PM – 2:15 PM in Eastern Time (ET).

Record-breaking Insulin Safety Week unites over 800 healthcare sites
More than 800 healthcare sites across the UK and Ireland signed up to take part in last week’s Insulin Safety Week, marking a record-breaking year for the national campaign.

New continuous glucose monitor launches in the UK
A new ‘next-generation’ continuous glucose monitor (CGM) by Chinese manufacturing giant Yuwell is now available in the UK.

Record-breaking Insulin Safety Week unites over 800 healthcare sites
More than 800 healthcare sites across the UK and Ireland signed up to take part in last week’s Insulin Safety Week, marking a record-breaking year for the national campaign.

NeedleBay supports Insulin Safety Week 2025 with real-life success story
Retired paramedic Paul Thompson credits an innovative device with transforming his diabetes management.

New CareSens Air continuous glucose monitor transforms diabetes management for busy mum
A busy mum with type 1 diabetes says the revolutionary CareSens Air continuous glucose monitor (CGM) has given her the freedom to manage her condition effortlessly.

JBDS seeks insights from inpatient diabetes teams to support safer EHR implementation
The Joint British Diabetes Societies (JBDS) is calling on inpatient diabetes teams across the UK to share their experiences of working with Electronic Health Records (EHRs) to help shape a new national resource.

Company behind diabetes management breakthrough sponsors Insulin Safety Week 2025
The company behind a pioneering device that significantly improves diabetes self-management will sponsor next month’s Insulin Safety Week 2025.

St Helens and Whiston achieve first DCAP accreditation!
Congratulations to St Helens and Whiston, the first inpatient diabetes service in the UK to achieve Level 1 accreditation with the Diabetes Care Accreditation Programme (DCAP)!

